Rabies is preventable — but once symptoms begin, it is almost always fatal.
Rabies risk: what to do after a bite, scratch, or saliva exposure
Rabies is a viral infection transmitted through saliva from infected mammals. The decisive factor is timely post-exposure prophylaxis (PEP) and meticulous wound care.
Wash for 15 minutes
Start vaccine ASAP
Category III may need immunoglobulin
Travel hotspots: Bali, Thailand, India
Start here
If you are unsure: treat the exposure as urgent. Rabies PEP is time-sensitive and highly effective when started promptly.
Download the one-page PDF summary for offline use.
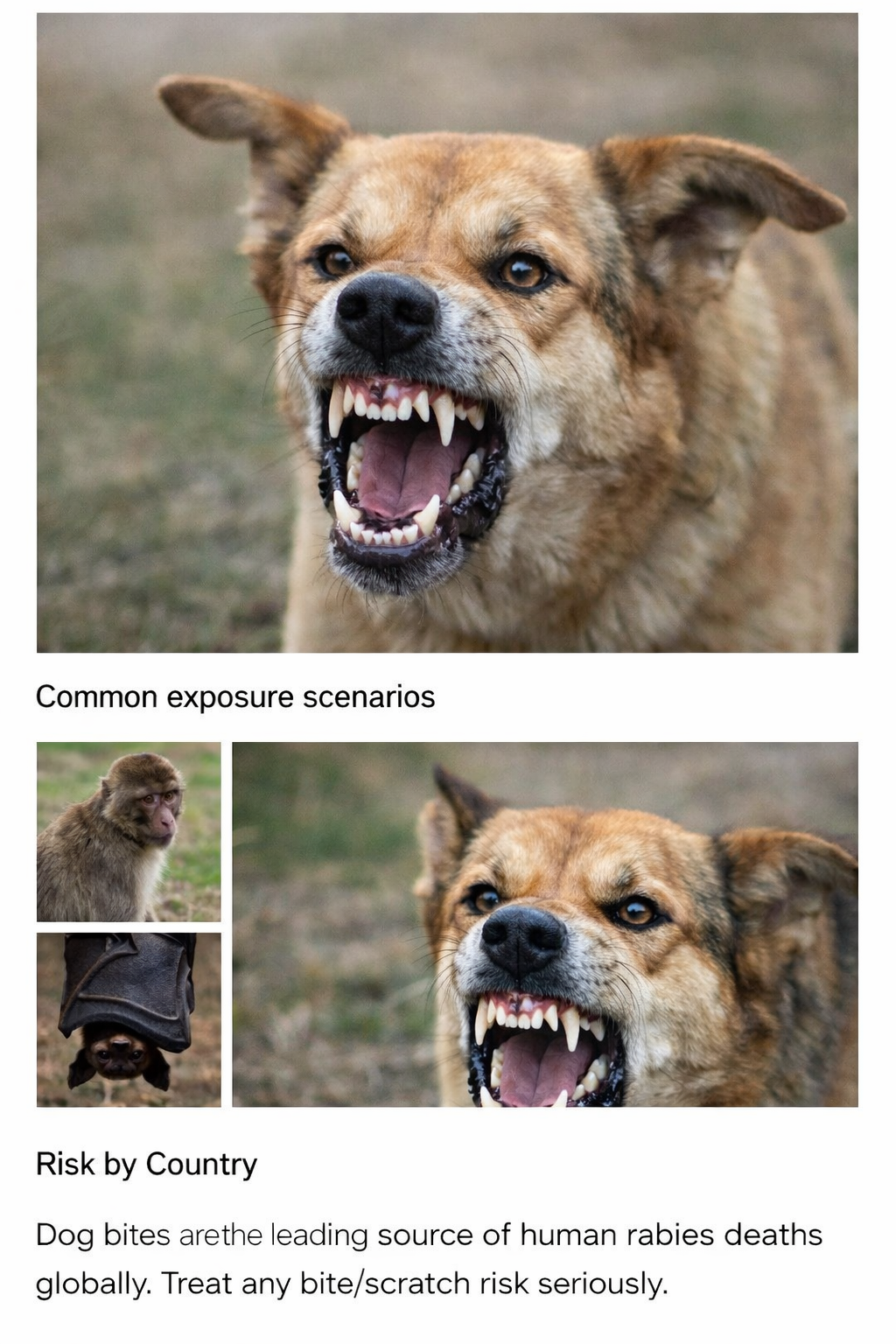
Download PDFCommon exposure scenarios
- Dog bite (most global human cases are dog-mediated)
- Cat bite or scratch (often underestimated)
- Monkey bite (tourist areas)
- Bat contact (even without a clear bite in some circumstances)

Why rabies is unique
Rabies can have a long and variable incubation period. The virus can travel via peripheral nerves toward the brain before symptoms appear.
Symptoms & outcomes
Once clinical rabies begins, outcomes are devastating, and mortality is close to 100% despite intensive care.
Travel and prevention
Pre-vaccination can simplify care after an exposure and is considered for higher-risk travel, long stays, or remote itineraries.